For some inexplicable reason, you watched the torture gore horror film
Hostel over the weekend. On Monday, you're having trouble concentrating at work. Images of severed limbs and bludgeoned heads keep intruding on your attempts to code or write a paper. So you decide to read about the making of
Hostel.You end up seeing pictures of the most horrifying scenes from the movie. It's all way too way much to simply shake off so then you decide to play
Tetris.
But a funny thing happens. The unwelcome images start to become less frequent. By Friday, the gory mental snapshots are no longer forcing their way into your mind's eye. The ugly flashbacks are gone.
Meanwhile, your parnter in crime is having similar images of eye gouging pop into his head. Except he didn't review the tortuous highlights on Monday, and he didn't play
Tetris. He continues to have involuntary intrusions of
Hostel images once or twice a day for the rest of the week.
This is basically the premise (and outcome) of a new paper in
Psychological Science by Ella James and colleagues at Cambridge and Oxford. It builds on earlier work suggesting that healthy participants who play
Tetris shortly after watching a “trauma” film will have fewer intrusive memories (
Holmes et al, 2009,
2010). This is based on the idea that involuntary “flashbacks” in real
post-traumatic stress disorder (PTSD) are visual in nature, and require visuospatial processing resources to generate and maintain. Playing
Tetris will interfere with consolidation and subsequent intrusion of the images,
at least in an experimental setting (
Holmes et al, 2009):
...Traumaflashbacks are sensory-perceptual, visuospatial mental images. Visuospatial cognitive tasks selectively compete for resources required to generate mental images. Thus, a visuospatial computergame (e.g. "Tetris") will interfere with flashbacks. Visuospatial tasks post-trauma, performed within the time window for memory consolidation [6 hrs], will reduce subsequent flashbacks. We predicted that playing"Tetris" half an hour after viewing trauma would reduce flashback frequency over 1-week.
The timing is key here. In the earlier experiments,
Tetris play commenced 30 min after the trauma film experience, during the
6 hour window when memories for the event are stabilized and consolidated. Newly formed memories are thought to be malleable during this time.
However, if one wants to extrapolate directly to clinical application in cases of real life trauma exposure (and this is problematic, as we'll see later), it's pretty impractical to play
Tetris right after an earthquake, auto accident, mortar attack, or sexual assault. So the new paper relies on the process of reconsolidation, when an act of remembering will place the memory in a labile state once again, so it can be modified (
James et al., 2015).
The procedure was as follows: 52 participants came into the lab on Day 0 and completed questionnaires about depression, anxiety, and previous trauma exposure. Then they watched a 12 min trauma film that included 11 scenes of
actual death (or threatened death) or serious injury (
James et al., 2015):
...the film functioned as an experimental analogue of viewing a traumatic event in real life. Scenes contained different types of context; examples include a young girl hit by a car with blood dripping out of her ear, a man drowning in the sea, and a van hitting a teenage boy while he was using his mobile phone crossing the road. This film footage has been used in previous studies to evoke intrusive memories...
After the film, they rated “how sad, hopeless, depressed, fearful, horrified, and anxious they felt right at this very moment” and “how distressing did you find the film you just watched?” They were instructed to keep a diary of intrusive images and come back to the lab 24 hours later.
On Day 1, participants were randomized to either the experimental group (memory reactivation +
Tetris) or the control group (neither manipulation). The experimental group viewed 11 still images from the film that served as reminder cues to initiate reconsolidation. This was followed by a 10 min filler task and then 12 min of playing
Tetris (the Marathon mode shown above). The game instructions aimed to maximize the amount of mental rotation the subjects would use. The controls did the filler task and then sat quietly for 12 min.
Both groups kept a diary of intrusions for the next week, and then returned on Day 7. All participants performed the Intrusion Provocation Task (IPT). Eleven blurred pictures from the film were shown, and subjects indicated when any intrusive mental images were provoked. Finally, the participants completed a few more questionnaires, as well as a recognition task that tested their verbal (T/F written statements) and visual (Y/N for scenes) memories of the film.
1The results indicated that the Reactivation +
Tetris manipulation was successful in decreasing the number of visual memory intrusions in both the 7-day diary and the IPT (as shown below).
modified from Fig. 1 (James et al., 2015). Asterisks indicate a significant difference between groups (**p < .001). Error bars represent +1 SEM.Cool little snowman plots (actually frequency scatter plots) illustrate the time course of intrusive memories in the two groups.
modified from Fig. 2 (James et al., 2015). Frequency scatter plots showing the time course of intrusive memories reported in the diary daily from Day 0 (prior to intervention) to Day 7. The intervention was on Day 1, and the red arrow is 24 hrs later (when the intervention starts working). The solid lines are the results of a generalized additive model. The size of the bubbles represents the number of participants who reported the indicated number of intrusive memories on that particular day. But now, you might be asking yourself if the critical element was
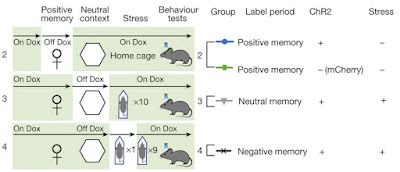
Tetris or the reconsolidation update procedure (or both), since the control group did neither. Not to worry. Experiment 2 tried to disentangle this by recruiting four groups of participants (n=18 in each)
— the original two groups plus two new ones: Reactivation only and
Tetris only.
And the results from Exp. 2 demonstrated that
both were needed.
modified from Fig. 4 (James et al., 2015). Asterisks indicate that results for the Reactivation + Tetris group were significantly different from results for the other three groups (*p < .01). Error bars represent +1 SEM. The No-Task Control and Tetris Only groups did not differ for diary intrusions (n.s.).The authors' interpretation:
Overall, the results of the present experiments indicate that the frequency of intrusive memories induced by experimental trauma can be reduced by disrupting reconsolidation via a competing cognitive-task procedure, even for established memories (here, events viewed 24 hours previously). ... Critically, neither playing Tetris alone (a nonreactivation control condition) nor the control of memory reactivation alone was sufficient to reduce intrusions... Rather, their combination is required, which supports a reconsolidation-theory account. We suggest that intrusive-memory reduction is due to engaging in a visuospatial task within the window of memory reconsolidation, which interferes with intrusive image reconsolidation (via competition for shared resources).
Surprisingly (perhaps), I don't have anything negative to say about the study. It was carefully conducted and interpreted with restraint. They don't overextrapolate to PTSD. They don't use the word “flashback” to describe the memory phenomenon. And they repeatedly point out that it's “experimental trauma.” I actually considered reviving
The Neurocomplimenter for this post, but that would be going too far...
Compare this flattering post with
one I wrote in 2010, about a related study by the same authors (
Holmes et al.. 2010). That paper certainly had a modest title:
Key Steps in Developing a Cognitive Vaccine against Traumatic Flashbacks: Visuospatial Tetris versus Verbal Pub Quiz.
Cognitive vaccine. Traumatic. Flashbacks. Twelve mentions of PTSD. This led to ridiculous headlines like
Doctors Prescribing 'Tetris Therapy'.
Here, let me fix that for you:
Tetris Helps Prevent Unpleasant Memories of Gory Film in Happy PeopleMy problem wasn't with the actual study, but with the way the authors hyped the results and exaggerated their clinical significance. So I'm pleased to see a more restrained approach here.
The media coverage for the new paper was generally more accurate too:
Can playing Tetris reduce intrusive memories? (Medical News Today)
Moving tiles as an unintrusive way to handle flashbacks (Medical Express)
Intrusiveness of Old Emotional Memories Can Be Reduced by Computer Game Play Procedure (APS)
But we can always count on the
Daily Mail for a good time:
Could playing TETRIS banish bad memories? Retro Nintendo game 'reduces the risk of post-traumatic stress disorder'2Gizmodo is a bit hyperbolic as well:
Tetris Blocks Flashbacks of Traumatic Events Lodged in the Brain [“lodged in the brain” for all of 24 hrs]
Questions for Now and the FutureIs there really nothing wrong with this study?? Being The Neurocritic, I always have to find
something to criticize... and here I had to dig through the Supplemental Material to find issues that may affect the translational potential of
Tetris-based interventions.
- The Intrusion subscale of the Impact of Event Scale (IES-R) was used as an exploratory measure, and subject ratings were between 0 and 1.
The Intrusion subscale consists of 8 questions like “I found myself acting or feeling like I was back at that time” and “I had dreams about it” that are rated from 0 (not at all) to 4 (extremely). The IES-R is given to people after distressing, traumatic life events. These individuals may have actual PTSD symptoms like flashbacks and nightmares.
In Exp. 1, the Reactivation +
Tetris group (M = .68) had significantly lower scores (p = .016) on Day 7 than the control group (M = 1.01). BUT this is not terribly meaningful, due to a floor effect. And in Exp. 2 there was no difference between the four groups, with scores ranging from 0.61 to 0.81.
3As an overall comment, watching a film of a girl getting hit by a car is not the same as witnessing it in person (obviously). But this real-life scenario may be the most amenable to
Tetris, because the witness was not in the accident themselves and did not know the girl (both of which would heighten the emotional intensity and vividness of the trauma, elements that transcend visual imagery).
It's true that in PTSD, the involuntary intrusion of trauma memories (i.e., flashbacks) have a distinctly sensory quality to them (
Ehlers et al. 2004). Visual images are most common, but bodily sensations, sounds, and smells can be incorporated into a multimodal flashback. Or could occur on their own.
- The effectiveness of the Tetris intervention was related to game score and self-rated task difficulty.
This means that
people who were better at playing Tetris showed a greater decrease in intrusive memories. This result wasn't covered in the main paper, but it makes you wonder about cause and effect. Is it because the game was more enjoyable for them? Or could it be that their superior visual-spatial abilities (or greater game experience) resulted in greater interference, perhaps by using up more processing resources? That's always a dicey argument, as you could also predict that better, more efficient game play uses
fewer visual-spatial resources.
An interesting recent paper found that individuals with PTSD (who presumably experience intrusive visual memories) have worse allocentric spatial processing abilities than controls (
Smith et al., 2015). This means they have problems representing the locations of environmental features relative to each other (instead of relative to the self). So are weak spatial processing and spatial memory abilities
caused by the trauma, or are weak spatial abilities a vulnerability factor for developing PTSD?
- As noted by the authors, the modality-specificity of the intervention needs to be assessed.
Their previous paper showed that the effect was indeed specific to
Tetris. A verbally based video game (
Pub Quiz) actually
increased the frequency of intrusive images (
Holmes et al., 2010).
It would be interesting to disentangle the interfering elements of
Tetris even further. Would any old mental rotation task do the trick? How about passive viewing of
Tetris blocks, or is active game play necessary? Would a visuospatial
n-back working memory task work? It wouldn't be as fun, but it obviously uses up visual working memory processing resources. What about
Asteroids or
Pac-Man or...?
4This body of work raises a number of interesting questions about the nature of intrusive visual memories, traumatic and non-traumatic alike. Do avid players of action video games (or
Tetris) have fewer intrusive memories of past trauma or trauma-analogues in everyday life? I'm not sure this is likely, but you could find out pretty quickly on Amazon Mechanical Turk or one of its
alternatives.
There are also many hurdles to surmount before
Doctors Prescribe 'Tetris Therapy'. For instance, what does it mean to have the number of weekly
Hostel intrusions drop from five to two? How would that scale to an actual trauma flashback, which may involve a fear or panic response?
The authors conclude the paper by briefly addressing these points:
A critical next step is to investigate whether findings extend to reducing the psychological impact of real-world emotional events and media. Conversely, could computer gaming be affecting intrusions of everyday events?
A number of different research avenues await these investigators (and other interested parties). And
— wait for it — a clinical trial of
Tetris for flashback reduction has already been completed by the investigators at Oxford and Cambridge!
A Simple Cognitive Task to Reduce the Build-Up of Flashbacks After a Road Traffic Accident (SCARTA)
Holmes and colleagues took the consolidation window very seriously: participants played
Tetris in the emergency room within 6 hours of experiencing or witnessing an accident. I'll be very curious to see how this turns out...
Footnotes1 Interestingly, voluntary retrieval of visual and verbal memories was not affected by the manipulation, highlighting the uniqueness of flashback-like phenomena.
2 It does no such thing. But they did embed a video of Dr. Tom Stafford explaining why Tetris is so compelling...
3 The maximum total score on the IES-R is 32. The mean total score in a group of
car accident survivors was 17; in
Croatian war veterans it was 25. At first I assumed the authors reported the total score out of 32, rather than the mean score per item. I could be very wrong, however. By way of comparison, the mean item score in
female survivors of intimate partner violence was 2.26. Either way, the impact of the trauma film was pretty low in this study, as you might expect.
4 OK, now I'm getting ridiculous. I'm also leaving aside modern first-person shooter games as potentially too traumatic and triggering.
ReferencesEhlers A, Hackmann A, Michael T. (2004).
Intrusive re-experiencing in post-traumaticstress disorder: phenomenology, theory, and therapy.
Memory 12(4):403-15.
Holmes EA, James EL, Coode-Bate T, Deeprose C. (2009).
Can playing the computer game "Tetris" reduce the build-up of flashbacks for trauma? A proposal from cognitive science.
PLoS One 4(1):e4153.
Holmes, E., James, E., Kilford, E., & Deeprose, C. (2010). Key Steps in Developing a Cognitive Vaccine against Traumatic Flashbacks: Visuospatial Tetris versus Verbal Pub Quiz. PLoS ONE, 5 (11) DOI: 10.1371/journal.pone.0013706James, E., Bonsall, M., Hoppitt, L., Tunbridge, E., Geddes, J., Milton, A., & Holmes, E. (2015). Computer Game Play Reduces Intrusive Memories of Experimental Trauma via Reconsolidation-Update Mechanisms. Psychological Science DOI: 10.1177/0956797615583071Smith KV, Burgess N, Brewin CR, King JA. (2015).
Impaired allocentric spatialprocessing in posttraumatic stress disorder.
Neurobiol Learn Mem. 119:69-76.